- Home
- slideshows
- miscellaneous
- Therapy in a pill: Breaking down the science behind the strange, surreal world of Netflix's "Maniac"
Therapy in a pill: Breaking down the science behind the strange, surreal world of Netflix's "Maniac"
In the show, participants in the trial get tested for defense mechanisms. Those tests are actually used to screen for mental illness.

In the show, the three pills are designed to replace cognitive-behavioral therapy. Here's what that really is.
In real life, cognitive-behavioral therapy (CBT) is often used to relieve symptoms of trauma, grief, or PTSD by helping patients understand their experiences and coping mechanisms. CBT can be used on its own or in conjunction with medication, and the aim is to return a sense of control, confidence, and predictability to patients' lives.
In the show, the characters' experiences when taking the pills parallels that process.
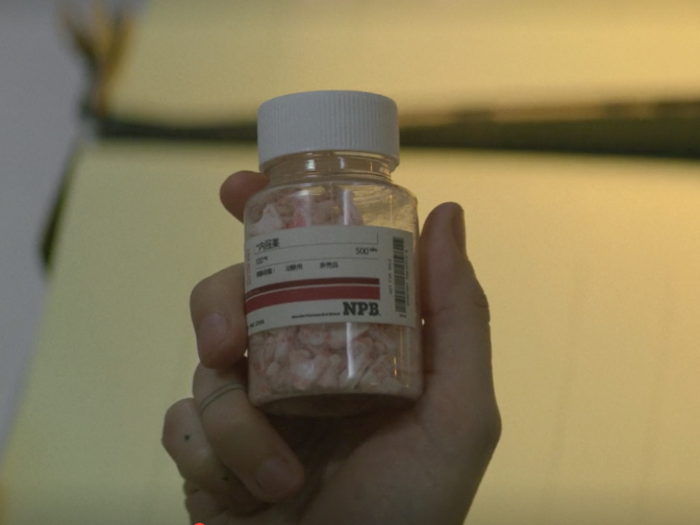
The first pill, A, stands for agonia, which means struggle in Greek. It's supposed to reveal and uncover a person's tragic experiences, making the patient relive them. Immersion therapy and gradual exposure to traumatic memory is usually a first step in trauma-focused cognitive-behavioral therapy.
The B pill stands for behavioral, and it's supposed to tear down defense mechanisms and expose lies created by the mind. This mirrors a step in CBT that educates patients about their reaction to trauma exposure. The goal is to get someone to realize their true feelings and shed coping mechanisms .
The C pill stands for confrontation, and it's supposed to get the patient to come to terms with the truth. Here, they must accept their own shortcomings and the consequences of their behavior. From this point, they can start to change, move on, and connect with others. This mirrors the step in CBT in which caregivers help patients process trauma-related thoughts and beliefs and help patients reassert control over their situation.
Many elements of the characters' diagnoses are consistent with real-life conditions and symptoms.

In episode five, Dr. James K. Mantleray, the inventor of the pills, gives each character a personalized assessment and diagnosis. Here are the diagnoses given to Annie and Owen, what they mean, and how well they match up with real-life classifications of these disorders.
Annie is told she shows signs of borderline personality (among other things). As defined by the National Institute of Mental Health, patients suffering from borderline personality disorder have a tendency to act impulsively and struggle with personal relationships. They can experience intense episodes of anger, depression, and anxiety that lasts from a few hours to days. Patients also are prone to cut off communication with someone in anticipation of being abandoned, feel chronic emptiness, and have intense but unstable relationship with those close to them. This aligns with Annie's character and actions in the show.
Owen finds out he shows signs of paranoid schizophrenia. Schizophrenic patients often have delusions about someone spying on them or plotting against them, visual and auditory hallucinations, flat expression of emotion and voice tone, and reduced feelings of pleasure in everyday life, according to the National Institute of Mental Health.
Real psychiatric pharmaceutical trials are very different than the one depicted in "Maniac."

The sequence of drugs being tested in the show's pharma trial is supposedly the 73rd iteration, following a long string of failures. A real-life drug that failed in 73 rounds of human clinical trials would probably not fly with the FDA, especially if (spoiler alert) the trials caused some patients to become brain-dead.
In reality, clinicians are required to file an Investigational New Drug Application with the FDA and update the agency with safety and progress reports throughout the trial process. (Here are the full FDA requirements for clinical research.)
There are, however, 916 real trials going on right now for trauma- and stress-related disorders. That's according to ClinicalTrials.gov, a database of privately and publicly funded clinical studies going on around the world.
These trials are experimenting with a variety of treatment techniques, including drugs, cognitive and behavioral therapy, psychotherapy, motor interference, oxygen exposure, deep brain stimulation, virtual reality simulations, online support, and exercise.
Could a drug actually help treat trauma and other psychological disorders by rewiring the mind? Research into psychedelics seeks to answer that question (to some degree).
"The mind can be solved. Pain can be destroyed," Dr. James K. Mantleray promises in the show. But could a real drug replace therapy and erase trauma by altering patients' minds?
Besides antidepressants and other mood-stabilizing medications, psychedelic drugs may be the closest thing we have right now to the pills in the show.
Research has suggested that psilocybin (the hallucinogenic agent in mushrooms), ayahuasca, and LSD may help patients with anxiety and depression rewire connections in the brain. Such drugs have the potential to kill the ego, which is responsible for erecting defense mechanisms.
"In the depressed brain, in the addicted brain, in the obsessed brain, it gets locked into a pattern of thinking or processing that's driven by the frontal, the control center, and they cannot un-depress themselves," David Nutt, director of the neuropsychopharmacology unit at Imperial College London, told Business Insider in 2017. "Psychedelics disrupt that process so people can escape."
MDMA, a psychoactive compound also known as ecstasy or molly, has also gotten attention in the past couple of years for its potential to treat patients with PTSD. In fact, the FDA granted a special designation that could fast-track its approval for that purpose.
"MDMA can act as a catalyst to make the therapy go faster, be more efficient, be deeper, get to that malignant thing that needs to be taken out and examined in a more sort of peaceful environment with more acceptance," psychiatrist Julie Holland said at a London conference on the science of psychedelics in 2017.
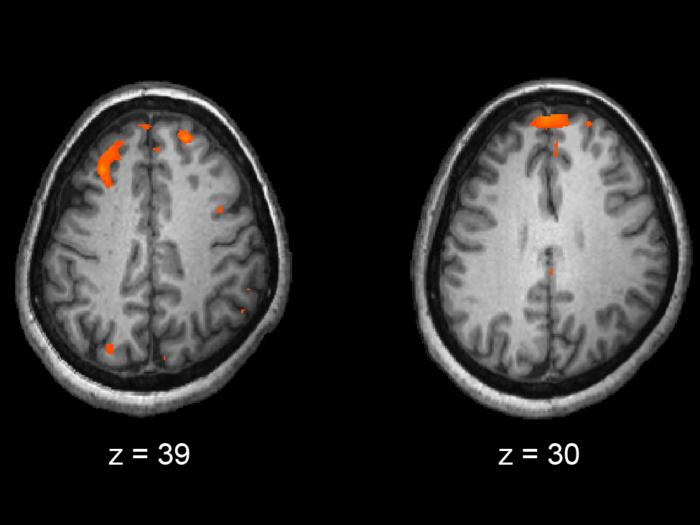
A computer in the show relays patents' brain activities to doctors. Machines we use today can perform the same functions.

During the trial in the show, researchers monitored the subjects' progress via a futuristic brain scan.
Although different than the technology depicted in "Maniac," functional magnetic resonance imaging (better known as fMRI scans) can be used for a similar purpose. The technology has been able to measure dream activity as well as activity in brain areas associated with emotion, movement, and decision-making.
Electroencephalography, or EEG, is also used to measure electrical activity in the brain.
So theoretically, it could be possible to use one of these machines to track a patient's mental journey.
The researchers in the show also use a computer program called GRTA to guide patients through their experience on the pills, kind of like an artificially intelligent therapist.
The closest real-life version of that may be AI therapy chatbots. But those algorithms are based on fairly simple computer codes, and they don't contain an "empathy program" like GRTA, so wouldn't become sentient or psychotic.
Temporary, hysterical blindness is a real condition.

In episode 9, during a climactic moment in the show, Dr. James K. Mantleray experiences temporary, dramatic, and hysterical blindness as a result of intense stress and anxiety.
In reality, neural messages from the retina can and do get lost along the transmission pathway to the processing center in rare cases.
High levels of emotional stress, for example, can cause blood pressure to rise and blood vessels near the eye to constrict, resulting in temporary vision loss. The rare condition, called amaurosis fugax, can be caused by migraines and other physical health conditions, stress from physical exercise, and even sexual intercourse.
Popular Right Now
Popular Keywords
Advertisement