- Home
- slideshows
- miscellaneous
- The coronavirus is set to push the US healthcare system to its limits - here are 8 things that hospitals risk running out of, from masks to ventilators
The coronavirus is set to push the US healthcare system to its limits - here are 8 things that hospitals risk running out of, from masks to ventilators
Medical providers are running out of protective gear like masks and gowns.

As the pandemic ramped up, the US struggled with shortages of COVID-19 tests.

As the coronavirus became more widespread, the country's healthcare system wasn't able to test many people suspected of having the virus.
As of March 8, the US had the lowest rate of coronavirus testing per capita of any developed country.
And the tests patients are getting often take days to come back, leaving patients with suspected cases in limbo.
That's starting to change as more automated ways to run the tests have started coming online, ideally speeding up the time it takes to get a result and the amount of tests labs can do. Some organizations are exploring at-home testing as well.
The US also faces a shortage of the materials used to run the COVID-19 tests.

We're also facing shortages of the chemicals that are critical to the process of running the coronavirus tests in labs.
CDC Director Robert Redfield told Politico in March that he was not sure if labs were stocked with enough of the materials used to extract the genetic material of the viruses present in a patient's sample.
"I'm confident of the actual test that we have, but as people begin to operationalize the test, they realize there's other things they need to do the test," Redfield told Politico.
Before a laboratory can conduct a coronavirus test, it first needs to extract RNA from the virus samples taken from patients.
This extraction requires a separate kit, and without that kit, researchers can't perform a coronavirus test.
Qiagen, a Netherlands-based company that makes the RNA-extracting kits, has said it's ramping up production of its RNA extraction kits in response to the shortage.
The swabs used to collect samples for the tests are starting to run out.
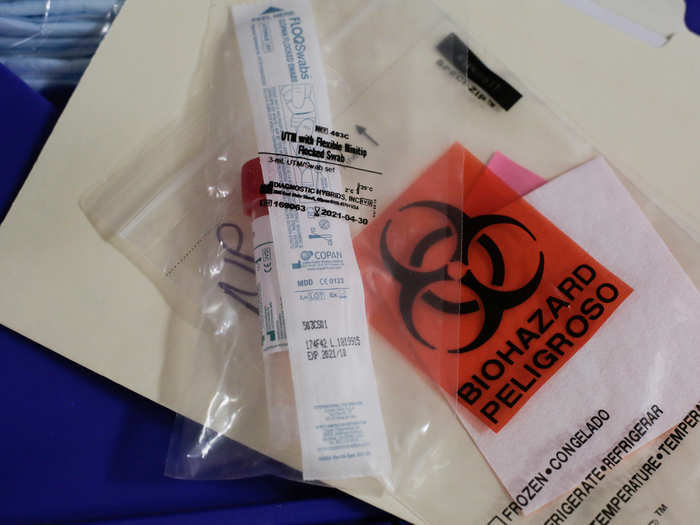
Politico reported Monday that we're starting to run out of the cotton swabs used to collect samples from patients.
The swabs are used to collect samples of patient's phlegm and saliva for testing.
Politico reported that the FDA recently approved more types of cotton swabs used for collection, though labs might still need help getting their hands on more.
Flu swabs are also at risk of falling into shortage, as doctors turn to the tests as a way to screen out patients who present with flu-like symptoms before they get the COVID-19 test, Dr. J.D. Zipkin, the associate medical director at Northwell Health — Go Health told Business Insider.
The US could face shortages of crucial medicines like antibiotics and a heart drug because of the coronavirus.

As early as February, the US started to face drug shortages caused by the coronavirus pandemic.
On February 27, the US Food and Drug Administration said it had identified the first drug shortage caused by the outbreak's effect on the supply chain for pharmaceuticals. The FDA said at the time it's identified 20 other drugs that rely on ingredients or final products from China, where the novel coronavirus has been spreading, but didn't name them.
Concerns of what shortages might mean for medical care in the US are now front and center. Much of the world's supply of generic drugs relies on ingredients made in China, and some factories have shut down in an effort to curb the coronavirus outbreak.
Additionally, India said in March that it is restricting the export of 26 drugs and ingredients to ensure it has supplies of key drugs like antibiotics, which could further limit supplies of medications to the US.
Italy, which has been hit hard by the coronavirus pandemic, is also responsible for making up a large supply of the world's active pharmaceutical ingredients.
Should shutdowns persist, they could prevent supplies for key drugs like antibiotics and the heart drug heparin from reaching generic drugmakers and ultimately patients around the world, experts told Business Insider.
Medical gear like ventilators could be in short supply.

Ventilators are a key resource for treating respiratory illnesses like COVID-19, the disease caused by the novel coronavirus. They're machines designed to help patients breathe if they're having trouble or can't on their own.
But there's a limited supply in the country, though some are available as part of a national stockpile that also includes protective equipment.
New York Governor Andrew Cuomo has warned that the state needs more ventilators and other equipment.
As hospitals start to see more patients, beds will be in short supply.

The US has fewer hospital beds per 1,000 people compared to places like Japan, South Korea, and Italy that have also been hit hard by the virus.
Not all beds are necessarily created equal. Right now, hospitals need special rooms that can isolate people with contagious diseases like the coronavirus, known as negative pressure rooms. And intensive care unit rooms, where doctors provide advanced life-saving care, are also in demand amid the pandemic.
"There's beds, and then there's ICU beds in a negative pressure room," said Soumi Saha, a senior director of advocacy at Premier, which works with hospitals around the US.
To increase capacity, she said, EvergreenHealth in Kirkland, Washington, an early epicenter of the US COVID-19 outbreak, put 58 patients in 15 negative pressure rooms that typically hold one patient each. Premier is set to survey the hospitals it works with to get a sense of how much added ICU capacity each is able to make in light of the outbreak beyond their normal capacities.
Elsewhere, hospitals are starting to cancel elective procedures.
To Jenna Mandel-Ricci, the vice president of legal and regulatory affairs for the Greater New York Hospital Association, it's a sign that hospitals aren't doing business as usual any more.
"It's the equivalent of me being like, 'In this response I can't do any other work except this" Mandel-Ricci told Business Insider.
Dr. Craig Coopersmith, interim director of the Emory Critical Care Center, oversees 300 ICU beds. He told Business Insider in March that many ICUs around the country are full on any given day.
While hospitals can cancel surgeries and take other measures to free up space, a spreading coronavirus outbreak would stretch them to their limits, he said.
Medical staff will be pushed to their limits.

Of course, a big limiting factor will be people.
Even if there's enough space or supplies, if hospitals don't have enough staff on hand — either because the workers have been exposed, are out sick, or even if they need to stay home with their kids, it could limit the amount of care hopsitals are able to provide.
"You need people to run the ventilators," Dr. Matthew Wynia, the director of the Center for Bioethics and Humanities at the University of Colorado Anschutz Medical Campus said.
One nurse who spoke to Business Insider already reported staffing shortages at her hospital. Nurses also face the potential of not getting paid if they become sick while treating patients amid the pandemic.
"I don't think America knows how much is at stake for us," Carmen Martinez, a nurse working in a California hospital told Business Insider's Allana Akhtar.
Popular Right Now
Popular Keywords
Advertisement