- Home
- slideshows
- miscellaneous
- Inside Lab100's 'clinic of the future': Mount Sinai's, cutting edge, new space to treat patients
Inside Lab100's 'clinic of the future': Mount Sinai's, cutting edge, new space to treat patients
"In order for Lab100 to work, we had to put the patient at the center of the design process," said Noah Waxman, the founder of Cactus, a design studio which helped create the Lab100 space.

Lab100 went from concept to launch over a 10 month period. It has been in private beta, or internal testing mode since October 2017.

Despite the heavy use of technology to run the clinic, the design team made sure to incorporate it in an elegant and seamless way.
The stations currently in the clinic are permeable to change.
"By definition, no one knows what the future of healthcare is, and neither do we. We made our best initial guess, recognizing that we're going to change based on the data we collect," said Stark. "It may turn out that we jettison some of these stations and put in additional stations."
The entire clinic is built like a stage set, explained Waxman. The panels are built on a easily-reconfigurable grid system so that machines and technology can be taken out and replaced without it looking like an after-thought.
Before stepping foot into the clinic, patients create profiles, complete a set of online surveys, and decide if they want to consent to research.
The surveys include information about your general medical history, nutrition, physical activity, mental health and sleep. These online surveys are used as an upgraded replacement for the usual clipboard surveys found in the doctor's office.
When a patient consents to research, Lab100 de-identifies the data, and makes it available to select researchers internally to power new discoveries.
The visit is 90 minutes and one-on-one. That means one patient to one physician. You start out at the first station in Lab100, which is a camera that takes your picture before the whole process begins.

This puts a face to your record throughout your visit and cuts down on medical errors. It also allows researchers to do more speculative work, where they can extract facial features using machine vision or computer vision and correlate those features to other health metrics being measured during the visit.
This is part of the idea that every bit of data collected at Lab100 has immediate clinical utility.
The second station takes your standard vital signs.

Your temperature, height, weight, blood pressure, heart rate and pulse oxygen levels are all taken here.
The equipment for measuring vital signs are standard, but the measurements are automatically recorded and integrated into the patient's profile. A doctor or a nurse practitioner can view and display data onto screens from an iPad.
At this point, a nurse or doctor can sit down with the patient for the first 10 minutes and review the data collected from the online surveys.

"This is where we get a sense of the patient's goals for the visit — what do they want to focus on, what's going well, what isn't going well," said Stark.
Lab100 worked with the Cactus design team to create its own in-house data visualizations that can educate the patient and give context around all the information collected about them. It allows them to learn and ask questions about what the numbers mean to their health.
The screen shows patients not only their data, but compares it to a population of their peers, with their approximate gender, age, race and ethnicity.
It will show you the range in which you blood pressure falls, for example, and if it's average, good or poor. If the patient comes back for repeat visits, Lab100 will also compare their current data to their past data.
The third station is the blood draw station. The material and procedure are pretty standard. The practitioner will do a veinous blood draw, and patients can watch a video in front of them during the blood draw.

The video is timed to preface you with information about why blood is a great analytic tools for assessing your health and treating disease. It then tells you a little bit about the technology Lab100 uses to analyze your blood and how that works.
Electrolyte, nutrient and cholesterol levels are measured, and your results will be available in 30 minutes.
It also tells you the possible research applications for your blood sample.
The blood analyzing lab is contained in a station where the patient can fully see what's going on behind the scenes.

The tiny machine used to analyze your blood sample contains a centrifuge and chemistry analyzer with a full-spectrum white light.
When you typically get your blood drawn in a hospital or a clinic, they're sending that blood to either the hospital's central lab, or an outside lab. These are large labs and results take a day or more to come back. Lab100 is deviating from that norm.
"We're trying to give patients more visibility, not only into their health, but into how healthcare happens with the hope that that visibility engages them as patients," said Stark.
At this point, every measurement taken in a conventional primary care visit has been covered.
The fourth station is a 3D full-body scanner.

Once the patient steps on this, it weighs them, and spins them around on the turntable. A depth-sensing camera takes a scan of the body and creates a high-resolution, 3D avatar.
The fifth station does body composition testing, akin to something you would find at a high-end health club or gym. It's not typically found in a doctor's office.

At the doctor's office, more traditional measurements like body mass index is used, which is a calculation of your weight divided by your height squared.
This machine does bioelectrical impedance analysis, which runs a small, electrical current through you to calculate the precise amount and distribution of water, fat, protein and mineral throughout the body. It also measures how muscle and fat are distributed across your body.
Once you step onto the platform, a video plays before you giving you information about what body composition is and how it plays a role in health.
After the video finishes, your data comes up on the screen. It can then tell you what percentile your measurements are in for your age, gender, race and ethnicity.

These results carry over from machine to machine until they're all cumulatively displayed on a huge screen at the end of your visit. On the backend, these results can also be used to calculate things like coronary vascular disease risks. These measurements can also let Lab100 tell patients how much interventions like diet and exercise can lower that risk.
The sixth station is a cognitive testing station.

Patients put on headphones and interact with an iPad, which tests vocabulary, processing speed, flexibility, episodic memory and attention.
The cognitive testing station also involves a dexterity test.
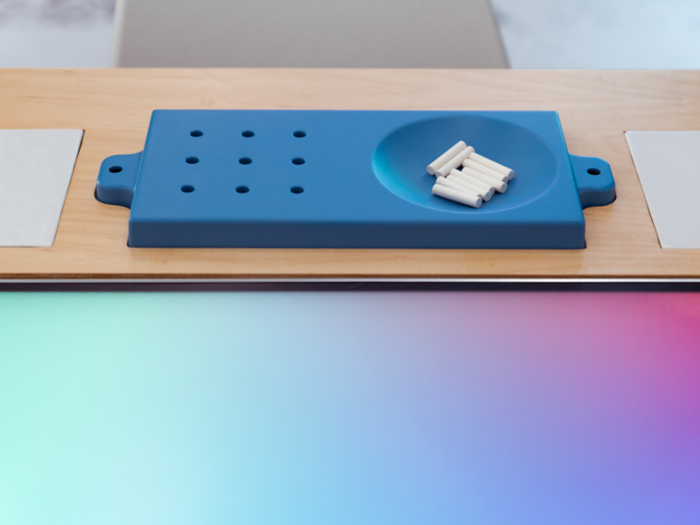
This is a traditional test called the pegboard dexterity test. It has only previously been used in the research realm because it's difficult to administer.
Working with the Cactus team, Lab100 found a way to more robustly collect this information. There is a video camera that records the patient's performance in a high frame-rate, high resolution footage. The hope is to extract more subtle features like hand tremors and use those to predict disease.
The seventh station is a strength testing station.

The tool Stark is holding tests grip strength, which is a correlate for overall body strength. It uses virtual reality as a way to incentivize the patient to give their maximum performance.
The last station tests balance.

An introduction video plays and explains Lab100's mission to use balance measurements from patients as a tool to address disease and optimize performance.
The station has two tools used to measure balance. There's the well-validated balance pod that the patient can step onto. An iPod with an onboard accelerometer is strapped to your waist, which helps measure sway as you try to stay as still as possible.
The team also repurposed the depth and movement sensing camera that comes with the Microsoft Connect as an additional balance measurement tool.

This camera has both range-finding ability and stereoscopics. It's also adept at finding human bodies and mapping their skeletons.
This is purely research-grade, said Stark, and it non-invasively measures sway. Stark said that it's likely this technology will become more commonplace in home theaters or TVs, and he wants to see if it can be used to non-invasively measure sway and gait, allowing more active detection of problems, especially in older adults.
As the visit draws to a close, the last 10 minutes are spend in front of a wide screen that stitches together all the measurements gathered throughout the visit.

"The idea here is not to obsess over every number, but to holistically look at what's going well, what isn't going well, and come away with one to three domains that you as the patient want to focus on," said Stark.
When patients leave the clinic, he aims for them all to have a specific action plan to implement. They can then schedule a follow-up in one to three months if they have a health issue to focus on, or six months to a year if they're healthy. And when they do come back, they'll have a chance to see how their metrics changed based on that intervention.
When you leave the clinic, you'll get a push notification on your phone and an email in your inbox telling you that your health report is available.

When you click the link, you can access your health report, where you can click in and get more details.
You can then print out the report, download it, or send it as a PDF to your physician or others.
A goal that Stark has in the next several month is to integrate data available on a person's smartphone like their steps or sleep pattern.
"There's a story to be told here about innovation within the incumbent. Mount Sinai to its great credit recognizes that as a large health system, it risks becoming a dinosaur very quickly if it can't figure out a way to keep up," said Stark. "One way to do that is to develop R&D shops and innovation organizations within."

At its heart, the clinic is still a research project. It's still working out some kinks and testing out variables like what populations this can best serve.
Lab100 is also partnering with other groups at Mount Sinai and externally to deploy components of the clinic elsewhere.
One example of that is their partnership with Mount Sinai's department of rehabilitation medicine to see if the Lab100 technology and infrastructure can be used to give a better assessment for sports performance or for patients who are aging with chronic disease.
Future applications could mean scaling parts of the operation down to the size of a self-service kiosk that could fit in a local pharmacy or virtualizing some of the components so that more tests are available on your mobile device or in your home. It could also mean partnering with other providers whether it's a health club, an employer, a pharmacy to deploy some of the components there.
Lab100 is expecting to launch to the general public in September or October of this year. But how will it live within the greater Mount Sinai health ecosystem?

The Lab100 prototype was never intended to be an at-scale operation, said Stark. "We're providing a high-touch experience so we can get good feedback and data from our patients and then we can take the learnings from this space and spin them outward into other clinical locations within Mount Sinai and beyond in the health system."
Lab100 is not a replacement for primary care. Rather, it serves as a complement. The vast majority of a typical primary care visit is spent on screening for, diagnosing and treating disease. By focusing on the preventative health side of the spectrum, Lab100 offers patients insight into the behavior and lifestyle determinants of health.
Occasionally, when medical findings are identified in Lab100, the team can refer patients within Mount Sinai and manage that hand-off so they're not just sending people back into the traditional healthcare system.
The team is also working closely with Mount Sinai's clinical information and IT teams to integrate Lab100 into the hospital's electronic health record, which is called Epic. All the data collected from the patient and the health report generated at the end will become part of the patient's Mount Sinai health record. That means Mount Sinai physicians can look back for your Lab100 report during future visits or check-ups.
"Ultimately our goal is to make this accessible to all," said Stark. "This is a project of our research institute, and we have a very strong interest in using this to make healthcare more affordable."
Popular Right Now
Popular Keywords
Advertisement