The Javits Center in New York City began COVID-19 vaccinations on January 13, 2021.Tayfun Coskun/Anadolu Agency/Getty Images
- Procuring a coronavirus shot may be easy or difficult, depending on where you live.
- A handful of states have managed speedy vaccine rollouts by attempting to deliver as many doses as possible or anticipating distribution challenges.
- Other states have struggled with technical glitches or lack of demand among healthcare workers.
Around 260 million Americans are eligible to receive coronavirus vaccines, but procuring a shot may be easy or difficult, depending on where they live.
US federal officials recommended Tuesday to expand vaccinations to all Americans ages 65 and older. Many states haven't finished vaccinating their first priority groups, which mainly include healthcare workers and nursing home residents. Some states have also prioritized vaccinations for frontline essential workers or individuals with health problems that raise their risk of severe disease.
Operation Warp Speed, the federal government's coronavirus vaccine initiative, recently advised states to vaccinate these priority groups in tandem in situations where vaccine supply exceeds demand or doses might expire. Warp Speed officials have also pushed states to begin deploying vaccines at pharmacies, community health centers, and mass vaccination sites.
That's a daunting challenge for many states with understaffed or underfunded health departments - though an $8.7 billion coronavirus relief package will soon assist states with vaccine distribution issues. States have also struggled to oversee mass vaccinations while simultaneously dealing with an unprecedented surge of coronavirus cases that has overwhelmed hospitals.
Here are the states where it's easiest and most difficult to get a shot, based on the number of doses administered per capita.
West Virginia leads the country in vaccinations per capita. As of Monday, none of the state's doses were sitting on shelves.
West Virginia Gov. Jim Justice.
Chris Jackson, File/AP Photo
West Virginia Gov. Jim Justice told CNBC on Monday that 100% of the state's vaccine supply was either in people's arms or had been tagged for a specific individual who would receive the shot in the coming days.
The state has also vaccinated all of its nursing home residents and staff, as well as those in assisted living, Justice said. That's because West Virginia didn't rely on a federal partnership with CVS and Walgreens to start vaccinating these individuals on December 21. Instead, it partnered with local pharmacies and deployed its National Guard to get nursing home vaccinations underway about five days earlier.
The state is also offering 14 vaccination clinics this week for individuals 70 and older. The first of these clinics opened on January 7.
As of Wednesday, West Virginia had administered more than 6,600 doses for every 100,000 people, according to data from the US Centers for Disease Control and Prevention.
South Dakota has administered 6,100 doses for every 100,000 people.
Technicians sort doses of the Pfizer-BioNtech vaccine.
Win McNamee/Getty Images
Around 4.5% of the state's population had been vaccinated as of Wednesday. So far, South Dakota has prioritized vaccinations for healthcare workers, nursing home residents, law enforcement, and correctional officers, but the state plans to extend vaccines to residents over 80 starting January 18. From there, it will open up doses to people 65 and older.
Health officials have attributed the state's successful rollout to strong partnerships with local stakeholders, including three major health systems: Avera, Monument, and Sanford.
"We sat down with the other healthcare systems and the state of South Dakota and mapped out — county by county — which system is vaccinating which county," Dr. Mike Wilde, chief medical officer at Sanford, told The Mercury News.
Alaska was quick to vaccinate elderly residents after a shortage of demand among healthcare workers.
Plastic surgeon Daniel Suver receives the Pfizer-BioNtech COVID-19 vaccine on December 16, 2020 at Providence Alaska Medical Center in Anchorage, Alaska.
Loren Holmes/Anchorage Daily News via AP, Pool
Alaska opened up vaccination clinics for healthcare workers at the end of December — only to find that there were appointments left over after a few days. The state took it as a sign to move on to its next priority group: people age 65 and older.
"We just said, 'OK, let's keep moving forward,'" Dr. Anne Zink, the state's chief medical officer, told Alaska Public Media.
Starting January 6, Alaska began allowing people 65 and older to sign up for appointments online. Many of the state's vaccine providers have registered with PrepMod, a website that connects residents to local vaccination sites.
Appointments for elderly residents in Alaska have been ongoing since Monday. The state has administered 5,800 doses for every 100,000 residents so far.
North Dakota's vaccine rollout benefited from early planning.
Dr. Avish Nagpal, an infectious disease specialist, receives the first shot of the COVID-19 vaccine given in North Dakota on December 14, 2020.
Dave Kolpack/AP Photo
The state has administered more than 5,600 doses for every 100,000 people, even after receiving fewer doses than health officials had anticipated. In addition to shipping doses to hospitals, North Dakota also delivered them to healthcare providers straight away.
"We are able to break down COVID-19 vaccine shipments into smaller quantities to get vaccines to rural areas of the state, where many healthcare providers are located," the state's health department told Becker's Hospital Review.
The department added that "healthcare providers were trained regarding the COVID-19 vaccines before they were authorized for use in the United States, which allowed for vaccines to be administered immediately."
Like West Virginia, North Dakota also didn't rely on the federal government's partnership with CVS and Walgreens to vaccinate nursing home residents. Nearly 60% of the state's long-term care facilities didn't participate in the program, meaning they received their shots either directly from the state warehouse or through independent pharmacies and public-health agencies.
Warp Speed officials have also heralded the speedy rollout in Connecticut.
Dr. Ramkumar Sankaran receives the Moderna COVID-19 vaccine in Hartford, Connecticut on December 21, 2020.
Joseph Prezioso / AFP via Getty Images
Connecticut has administered around 4,800 doses for every 100,000 residents so far. The state finished administering the first round of shots to its 213 nursing homes and long-term-care facilities on January 8.
Local health officials say there are multiple reasons for Connecticut's successful rollout. One is seamless communication between hospitals and Gov. Ned Lamont's office, which engage in weekly calls. Hospitals have also helped one another by sharing doses if a facility falls short of demand, or finding healthcare workers to vaccinate if extra doses are available.
Josh Geballe, Connecticut's chief operating officer, told the Hartford Courant that the state is attempting to strike a balance between "micromanagement and the wild west." That means expanding vaccinations to first responders or residents ages 75 or older if there's a surplus of shots at the end of the day. Many of the state's vaccine providers keep a waitlist of these individuals so they can call upon them quickly to get vaccinated.
Starting Monday, Connecticut will begin vaccinating individuals 75 and older as part of its routine schedule. A state phone line will help coordinate appointments, but large healthcare systems are also being asked to reach out to residents and schedule appointments on their own.
Alabama's vaccine rollout, on the other hand, has fallen short. Fewer than 1,900 doses for every 100,000 residents have been given out so far.
A pharmacist prepares the Pfizer-BioNTech vaccine.
Jessica Hill/AP Photo
Alabama's public health officer, Dr. Scott Harris, told local news channel WRBL that the state's vaccine supply was actually smaller than had been reported by the federal government.
"We absolutely acknowledge that we need to be doing this faster. Although, I take issue with the numbers being reported," he said on Wednesday. "Alabama supposedly has allocation of 300-and-something-thousand doses. We have actually only received about 270,000 doses in our state."
The state also has a large rural population — around 45% of residents live in rural areas, making it difficult to find centralized locations to deliver shots.
"Administering a vaccine in rural Alabama is not about pulling up to a Walmart parking lot," John McGuinness, former state surgeon for the Alabama National Guard, told The Washington Post. "This amounts to a military campaign, moving from town to town and gathering demographics, relying on local leaders and being comprehensive in that way."
Georgia has also struggled to put shots into arms.
Emergency room nurse David Wilson receives the COVID-19 vaccine as Georgia Governor Brian Kemp, right, looks on outside the Chatham County Health Department on December 15, 2020 in Savannah, Georgia.
Sean Rayford/Getty Images
The state has administered less than a quarter of the doses it has received so far. For every 100,000 residents, only 2,200 doses have been given out.
Like Alabama, Georgia has run into issues with vaccinating residents in rural areas. Dr. Kathleen Toomey, commissioner of the Georgia Department of Public Health, told local news channel 11Alive that some residents were wary of taking the vaccine.
Staffing shortages at local hospitals may have further slowed the vaccination process.
Georgia also ran into technical issues when it opened up appointments to people 65 and older on Monday. An online registration form for two counties, Cobb and Douglas, crashed. Phone lines jammed. And several district health departments were eventually forced to stop taking appointment requests.
South Carolina hospitals have encountered a lack of demand among healthcare workers.
South Carolina Gov. Henry McMaster shows a listing of hospitals in the state that have received the COVID-19 vaccine on January 5, 2021.
Jeffrey Collins/AP Photo
At the start of its vaccine rollout, South Carolina stipulated that 70% of eligible healthcare workers and nursing home residents needed to be vaccinated before moving on to the next priority groups. But by early January, local hospitals said not all healthcare workers were taking advantage of the available doses, and some vaccines appointments remained empty.
On January 5, Gov. Henry McMaster told healthcare workers they had 10 days to get a shot or "move to the back of the line."
South Carolina has administered fewer than 2,300 doses for every 100,000 residents, according to the CDC, but some hospital officials say that data could be behind.
Patrick Cawley, vice president for health affairs at the Medical University of South Carolina, told The State that the federal government's reporting system was slowing down his center's ability to record vaccinations in real time. Indeed, for many states, the number of reported vaccinations typically lags 24 to 72 hours behind those that have actually been administered.
Idaho planned for more doses than it received in December.
A nurse prepares a syringe of the COVID-19 vaccine.
Brian van der Brug/Los Angeles Times via AP, Pool
Out of every 100,000 Idaho residents, fewer than 2,400 doses have been given out. At that rate, it could take three years to vaccinate all of the state's 1.8 million residents.
With the pace of vaccinations starting to ramp up, state health officials estimate they can immunize about more than half of Idaho's population by the end of 2021.
But Idaho officials were thrown for a curve in December, when the state received far fewer doses than it had anticipated. Idaho's vaccine supply for the week of December 21 was cut by 44%. Gov. Brad Little urged residents at the time to "be patient with the distribution."
Technical glitches slowed down vaccination appointments in Arizona.
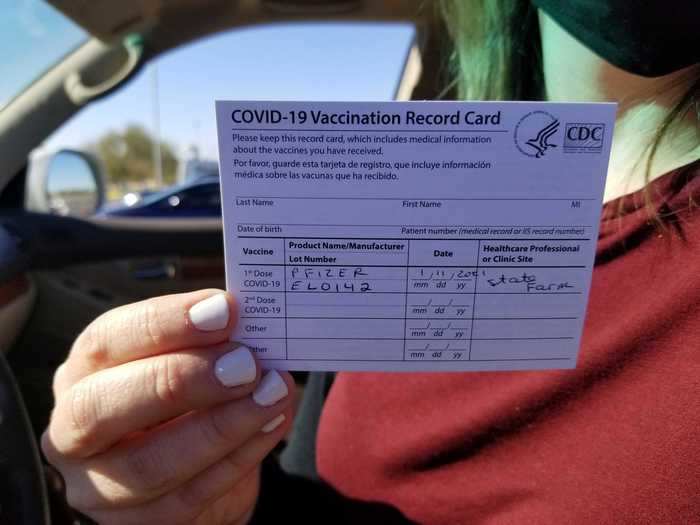
Emily Alexander, 37, shows her COVID-19 vaccination card shortly after getting the vaccine in the parking lot of the State Farm Stadium in Glendale, Arizona on January 11, 2021.
Terry Tang/AP Photo
Arizona ran into issues with scheduling appointments for healthcare workers at the start of its vaccine rollout. In Maricopa, the state's most populous county, the health department website directed residents to vaccination sites well outside their immediate area. The system also had trouble downloading insurance information or following up with individuals about their second doses.
County representatives told local radio station KJZZ that the error "slowed down the entire vaccine operation and put us days behind" in delivering shots.
Though the state has expanded its rollout to more priority groups, Arizona has administered fewer than 2,400 doses for every 100,000 residents. On Monday, residents said they were having trouble making appointments through the Arizona Department of Health Services website, likely due to heavy online traffic.
The state's healthcare system is also overburdened by a tsunami of coronavirus patients, meaning there aren't enough staffers to administer shots. By the end of December, NBC News reported, four out of five doses were sitting on shelves, waiting for someone to administer them.