Do ask which brand of COVID-19 vaccine is given to you, advises an expert Dr Vipin M. Vashishtha; that and 14 other questions that you may seek answers for
Kavita Majumdar

- “Both Covishield or Covaxin vaccines are going to have equal efficacy against the severe disease.”
- The government has advised not to administer Covishield vaccines to pregnant and lactating mothers.
- For people who have already been infected, the government advises that after 14 days of acute infection, a person can be vaccinated irrespective of his/her antibodies report.
- Check out the latest news and updates on Business Insider.
Business Insider approached Dr Vipin M. Vashishtha — who is currently the editor-in-chief at Indian Academy of Pediatrics (IAP) Textbook of Vaccines and former convener, IAP Committee on Immunization, plus he is also a consultant paediatrician at Mangla Hospital & Research Center, Bijnor, UP — to answer some of the other lingering questions we may have about the vaccine.
What are the different types of Covid-19 vaccines?

Basically, there are two types of vaccines: first, those developed on protein-based technique, and second, developed by gene-based technique/platform. Genetic platforms are more recent than the conventional protein-based techniques. A genetic material (nucleic acid) of the virus is used to produce proteins inside the cell in the former.
They are three types of vaccines:
a) Viral vector - where a harmless virus is used to carry a gene encoding the spike protein of SARS-CoV-2.
b) DNA - the gene encoding for spike protein is inserted in a bacterium that converts in the nucleus of a cell to mRNA and forms spike protein.
c) mRNA (a messenger RNA developed in a lab to carry instruction to form spike protein without entering the nucleus of the cell.
The live attenuated vaccines contain a genetically weakened virus that replicates to a limited extent, causing no disease but inducing immune responses similar to that induced by natural infection. The protein-based vaccines include inactivated (a killed virus is used as a vaccine), protein subunit (a part of the whole virus) and virus-like particle (only outer cover/shell of the virus) vaccines.
Are all Covid-19 vaccines equal? Which is the most efficacious vaccine candidate so far?

Not all vaccines are going to be successful, nor all are going to be equally efficacious against Covid-19 diseases. One vaccine by the University of Queensland was terminated because it yielded a false-positive HIV test in participants.
Most are found more efficacious against severe infections than against milder ones. This is more important as far as personal protection is concerned. In the phase III trials, the mRNA vaccines (by Pfizer and Moderna-94-95%) have far better efficacy than Gamaleya’s vector (91%) and Oxford’s vector vaccines (62%). Inactivated (killed) vaccines by China have lower efficacy ranging from 50-70%.
If one analyses the animal (macaque) trials, none of the key vaccines was able to prevent viral infection. However, all of them prevented severe disease. According to animal studies and early human trials, the highest number of antibodies were produced by Novavax followed by Moderna, Sinopharm and Janssen's vaccines, and lowest by Sinovac's killed vaccinates.
What about the safety of these vaccines?

In this case, vaccines with high efficacy are known to be least tolerable. For example, killed vaccines, though least efficacious, will be highly safe. As far as immediate, minor side effects and tolerability are concerned, this is in reverse order. Most efficacious vaccines like mRNA and vector vaccines may be more reactogenic - meaning they may produce more pain, fever, and tenderness. The killed vaccines have the least amount of these local side effects. We need long-term follow-ups to comment on rare, severe or critical adverse effects.
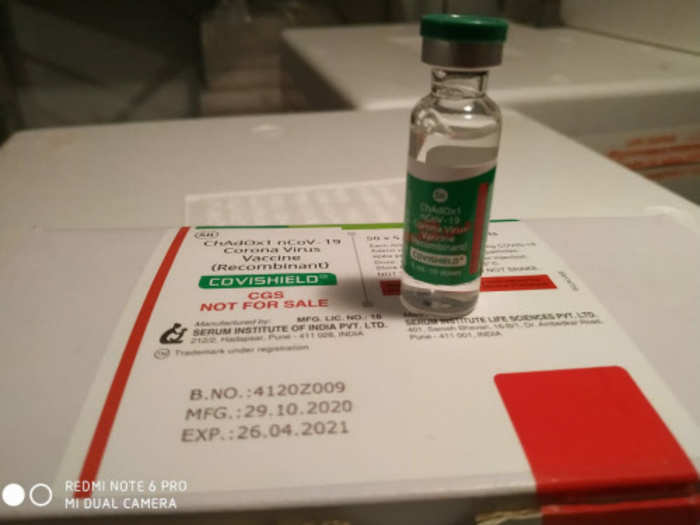
India is going to use two vaccines - Covishield by Serum Institute and Covaxin by Bharat Biotech. Which of the two vaccines is superior?

Both the vaccines are going to have equal efficacy against the severe disease. And this is the most important thing to note. It is true we do not know about the effectiveness of Covaxin since phase III study is still undergoing. It is expected to be around 50-60%. Covishield has shown 62% efficacy against Covid-19 and almost 100% against severe disease. However, as stated above, the local side effects (pain and fever) of the Covaxin is going to be lesser than Covishield since it is a killed vaccine.
However, the Government of India (GoI) has not given a prospective vaccine recipient a choice to select the vaccine. They will be immunised with whatever is offered to them by the government.
The GoI has advised 28 days (4 weeks) interval between two doses of both the vaccines. However, in the Covishield (Oxford’s) vaccine trial in the UK, it was seen that a longer interval (>6 weeks) results in better efficacy. What are your views?

Yes, it is true. In fact, if you go through the published trail of Covishield/Oxford vaccine in The Lancet, the single dose of the vaccine was found to have higher efficacy than two doses. And the longer interval, say around 8-12 weeks between the two doses resulted in higher efficacy. A longer interval between two doses usually results in better immunity. However, we need more data to decide the dose issue.
There are anxieties over future genome integrations and mutations with some Covid-19 vaccines. Are the concerns justified?

Broadly, two types of Covid-19 vaccines enter the human cell's nucleus. They include viral vector and DNA vaccines. However, DNA vaccines do not alter a person's DNA at all. They provide a temporary addition in a small number of cells. They do not enter the genome but merely imitate what happens when we get infected by a virus. A virus inserts its DNA into our cells to enable it to replicate and spread. And a vaccine must do that as well but in a controlled manner. Genetic material (DNA or RNA) from the virus is there inside our cells during a viral infection, but most viral infections do not then leave DNA that becomes part of the genome. However, in some instances, it happens. HIV, for example, has a "reverse transcriptase," which copies the viral genetic material back into the genome. But viruses like the coronavirus or influenza do not have that enzyme.
Will the current generation of vaccines be effective against a mutated variant?
The SARS-CoV-2 virus mutates regularly, acquiring about one new mutation in its genome every two weeks. In the UK variant, B117, there are 23 gene mutations, eight are in spike protein. The South Africa variant has three mutations in the receptor-binding domain (RBD) of the spike protein. The primary mutation is N501Y, a mutation in the RBD of the spike protein at position 501 that may make the receptor binding stronger. That would make South Africa's variant more dangerous.
Though the B117 strain is found to be 56% more transmissible than the older variant, no difference in the severity of Covid-19 disease was noted, and this variant’s susceptibility to current vaccines has also been established. In the case of the South Africa variant, there are some indications (mutation like E484K) that it may resist neutralisation by vaccines, but it is not uniform. And existing vaccines can still neutralise the virus by attacking other parts.
There is no need to panic. The current vaccines will be useful for quite a while. The virus will need to mutate much more and will take time to induce significant impact on vaccines. All the licensed vaccines are "polyclonal”, producing different antibodies and T-cells that target several spike proteins parts.
Can we see an influenza-like situation where the virus changes its structure every year?

It is difficult to say with certainty how the SARS-CoV-2 virus will behave later. Will it become endemic like influenza with seasonal low-intensity outbreaks or a common cold coronavirus causing mild disease only in children, we simply do not know now.
We may see an antigenic drift of SARS-CoV-2 and may need to update the vaccine's strain with some regularity. Even if significant changes occur in the RBD and a new strain emerges, the vaccines based on nucleic acid technology can be tweaked to tackle these mutants within a few weeks. A recent study suggests that Pfizer's vaccine is effective against new variant containing mutation N501Y, present in both UK and South Africa variants.
Should a person with a history of Covid-19 and still having antibodies in blood also be offered Covid vaccine?

We still do not know how long the immunity following a natural infection would last. But as discussed below, they can persist up to eight months following recovery. Further, out of >94 million infections, only around 40 cases of confirmed reinfections are documented. It means, largely, a natural infection provides protection to reinfection. If there is a shortage of vaccines, prioritisation can be attempted, and those with antibodies and history of infection in recent past (<3months) can be exempted of vaccination. However, the GoI has advised that after 14 days of acute infection, a person can be vaccinated irrespective of his/her antibodies report.
How long does the vaccine-induced protection against COVID-19 last?
As of today, nobody has the answer to this query. Most recent reports suggest that natural infections at least provide immunity to three to eight months. However, to get a concrete answer, the vaccinated subjects should be serially followed up for at least 1-2 years post-vaccination. So far, we have the efficacy data of only up to two-three months of follow up.
Would a single dose of a two-dose scheduled vaccine be effective?
Both Pfizer and Moderna vaccines may provide reasonable protection after the first dose. Data suggest significant protection even without a second shot. Moderna reported the efficacy of 1st dose to be 80.2% in preventing Covid-19 starting two weeks after the initial jab. For both vaccines, the sharp drop in disease in the vaccinated group started about 10-14 days after the first dose, before receiving the second. Similarly, the Covishield (Oxford) vaccine has shown significant efficacy after a single dose in the UK.
However, it is still not clear for how long the protection after a single dose will last. Pfizer has warned that they had no evidence that their vaccine will continue to protect against Covid-19 if the booster shot is given later than tested in trials.
How well will older individuals, who are most at risk from COVID-19, respond to the vaccine?

The data gathered so far suggests the Moderna vaccine works better in younger people. The vaccine efficacy (VE) was 95.6% for participants 18 to <65 years of age and 86.4% for participants 65 years of age and older. In 18-55 years old, the majority only show a slight decrease in antibodies in three months following their second dose. However, in 56-70 & 71+ age groups, the antibodies fall between 50 and 95%. This suggests that the duration of antibodies from the Moderna vaccine will be relatively short, potentially less than a year in older age groups. Oxford's group has not yet analysed their data in older age group people.
Will children also need Covid-19 vaccines?

Vaccination of kids will be required at the later stages. However, the new B117 variant has caused widespread disease in children that may necessitate vaccination of kids also. One important issue is tolerability of the new vaccines: Children usually show greater reactogenicity than adults. Many of the vaccine candidates have relatively strong side effects, low-dose vaccines might be needed for this age group, especially for viral vector and mRNA vaccines.
Will the current vaccines be given to pregnant women and lactating mothers?

No clinical trial of available vaccines has administered these vaccines to pregnant women and lactating mothers. Conventionally, the live viral vaccines are avoided in these categories. However, inactivated vaccines like Covaxin do not cause any adverse effects and can be given in these situations. The GoI has advised not to administer Covishield vaccines to pregnant and lactating mothers.
READ MORE ARTICLES ON
Popular Right Now
Popular Keywords
Advertisement