I spent a week in Uganda reporting on women's health - here's everything I learned
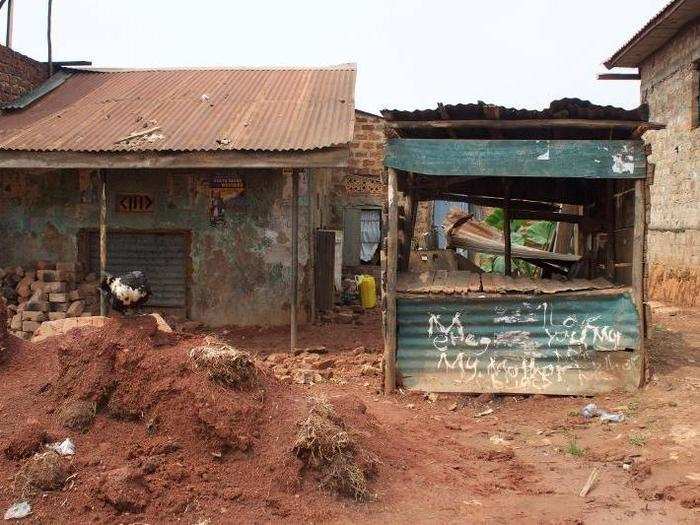
Sex work is a reality for many poor women in slum areas of Kampala, the capital city of Uganda. Moonlight Star Clinic, in the Bwaise area, was founded in 2007 specifically to offer services to sex workers.

The clinic helps around 600 sex workers each year, many from the Kimombasa slum area. It also expanded its services to 23,000 people in the community to reduce the stigma associated with sex work.

I was told that the women typically earn 500 Ugandan shillings (or $0.15 USD) for sex, which is less than half the cost of a pack of condoms.

I met with a 29-year-old sex worker with four children. She had been a sex worker for eight years, works every night, and rents a bed out of this brothel. That day, she had a bloody eye after being beat up by a customer.

I also met with a 28-year-old, who turned to sex work after her husband left her three years ago. She felt sex work was her only option, and this is how she provides for her six children.

Both women face the threat of violence daily. The clinic has services to help protect sex workers from violence, but it's hard to stay safe.
In the rural district of Luweero, which is about 50 miles north of Kampala, I learned that the average Ugandan woman gives birth to six children, though many want fewer than five.

The median age of first birth for Ugandan women is 18.9 years old. Most men and women know about birth control, but only 30% of married women are using contraception.

Butuntumula HCIII in Luweero is an outpost facility, which means it can provide basic health care and is run by nurses and midwives. These types of clinics are common in rural areas.

The clinic's midwives educate women and men on different contraceptive methods. Injectables are the most popular, used by 14% of married women and 18% of sexually active single women.

Ugandans face many barriers to family planning, including a lack of access and pervasive, misinformed beliefs that it causes cancer, increases promiscuity for women and leaves men impotent.

Nansubuga Gorreti, a 42-year-old mother of four in Luweero, faced similar barriers when she first wanted to go on birth control. Her husband blocked her from seeking out family planning, but after visiting the clinic, he was swayed, and she now uses injectables.

Dr. Agel Akii, a senior consultant OB/GYN at the Christa Medical Center in Jinja, Uganda, told me that cervical cancer screenings are becoming more popular among Ugandan women.

Most cervical cancer deaths are caused by the Human Papillomavirus (HPV). In Uganda alone, 3,500 women are diagnosed with cervical cancer each year, and 2,500 die. Dr. Akii (pictured, right) told me most women don't know about the link between HPV and cervical cancer.

Source: Aspire Africa
The OB/GYN explained that women know that cancer kills. Dr. Akii said women have been told to protect themselves against HIV with condoms, which should hopefully lower HPV transmission rates as well.

Women in rural areas often have to walk up to 18 miles to give birth at clinics, such as Lugasa HC III in Kayunga, nearly 40 miles north of Kampala.

Read more about the clinic here.
A number of health efforts, including outreach, in Uganda are led by international NGOs, such as Marie Stopes International.
Sometimes health workers are met with resistance from people who oppose family planning (largely men), but for the most part, these outreach efforts are appreciated within the community.

Learn more about a young community health advocate here.
All in all, the week I spent in Uganda was eye opening. There is a need for improvement, but there are also great people working hard to ensure that happens.

Popular Right Now
Popular Keywords
Advertisement